- Anatomy
- Conditions
- Procedures
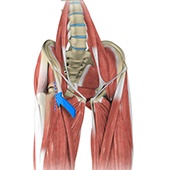
Anterior Hip Replacement
Direct anterior hip replacement is a minimally invasive hip surgery to replace the hip joint without cutting through any muscles or tendons as against traditional hip replacement that involves cutting major muscles to access the hip joint.
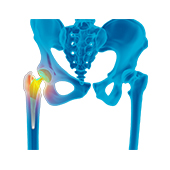
Revision Hip Replacement
During total hip replacement, the damaged cartilage and bone are removed from the hip joint and replaced with artificial components. At times, hip replacement implants can wear out for various reasons and may need to be replaced with the help of a surgical procedure known as revision hip replacement surgery.
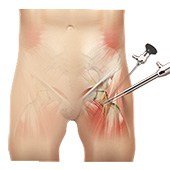
Hip Arthroscopy
Hip arthroscopy, also referred to as keyhole or minimally invasive surgery, is a procedure in which an arthroscope is inserted into your hip joint to check for any damage and repair it simultaneously. An arthroscope is a small, fiber-optic instrument consisting of a lens, light source, and video camera. The camera projects images of the inside of the joint onto a large monitor, allowing your surgeon to look for any damage, assess the type of injury and repair the problem.
Hip Labral Repair
Labrum is a ring of strong fibrocartilaginous tissue lining around the socket of the hip joint. Labrum serves many functions where it acts as a shock absorber, lubricates the joint, and distributes the pressure equally. It holds the head of the femur in place and prevents the lateral and vertical movement of the femur head within the joint. It also deepens the acetabular cavity and offers stability against femoral head translation..
Hip Reconstruction
Hip reconstruction is a surgery to repair or replace a damaged hip joint that causes pain and limits your movement.
Robotic Total Hip Replacement
Robotic total hip replacement is a minimally invasive procedure where your surgeon is assisted by a robotic system to perform a total hip replacement surgery.
Ultrasound Guided Hip Injections
An ultrasound scan is an imaging procedure that uses high-frequency sound waves to produce pictures of the inside of the body. Ultrasound-guided hip joint injections are used to diagnose the underlying cause and relieve hip pain. The injection consists of a special mixture of an anesthetic and a steroid that blocks pain impulses and reduces inflammation in the injected area.
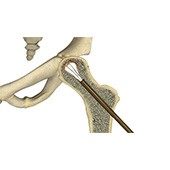
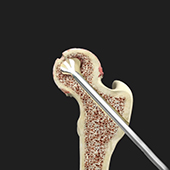
Hip Core Decompression
Core decompression is indicated in the early stages of avascular necrosis when the surface of the head is still smooth and round. It is done to prevent total hip replacement surgery, which is indicated for severe cases of avascular necrosis and involves the replacement of the hip joint with an artificial device or prosthesis.

 512-328-2663
512-328-2663